1.
Introduction
The COVID-19 epidemic has lasted for more than one year and caused more than three million deaths globally. More seriously, a second wave of COVID-19 epidemic in the northern hemisphere has emerged and caused a dramatic increase in COVID-19 cases and deaths [1]. Compared with the other continents, Africa has a relatively lower prevalence of COVID-19 [2]. However, the African-American population shows a higher COVID-19 susceptibility than the other U.S. populations [3]. It indicates that the genetic factor cannot explain the significantly lower prevalence of COVID-19 in African countries. To explore the factors that are potentially responsible for the significant difference in the prevalence of COVID-19 between African-Africans and African-Americans, we compared some factors associated with the COVID-19 epidemic between African countries and the U.S., including climate, demographic, underlying diseases, and smoking.
2.
Materials and methods
We collected the data of cumulative confirmed COVID-19 cases and deaths, temperature, humidity, wind speed, age distribution, incidences of age-related diseases, lung diseases, and HIV, and smoking rate for African-Africans in 40 African countries and for African-Americans in 50 U.S. states and New York city. The African-Americans refer to blacks Americans, the second largest minority population in the U.S. The numbers of cumulative confirmed COVID-19 cases and deaths were the records on September 3, 2020. The data of temperature, humidity, and wind speed were the records from January 1, 2020, to September 3, 2020. All data supporting the findings of this study are available within the paper and its supplementary information files (Tables S1 and S2).
Using the one-sided Mann–Whitney U test, we compared numbers of COVID-19 cases and deaths and several variables potentially associated with the prevalence of COVID-19 between African-Africans and African-Americans. These variables included the incidences of cardiovascular diseases, chronic kidney disease, chronic obstructive pulmonary disease (COPD), diabetes, HIV, hypertension, neoplasms, stroke, and tuberculosis, smoking rate, percentage of aged population (≥65 years), percentage of young population (<10 years), humidity, temperature, and wind speed. Moreover, we evaluated the Spearman correlations of COVID-19 cases and deaths with these variables. Besides, we ranked the importance of these variables in distinguishing the significantly different COVID-19 prevalence between African-Africans and African-Americans based on the chi-square statistic.
3.
Results
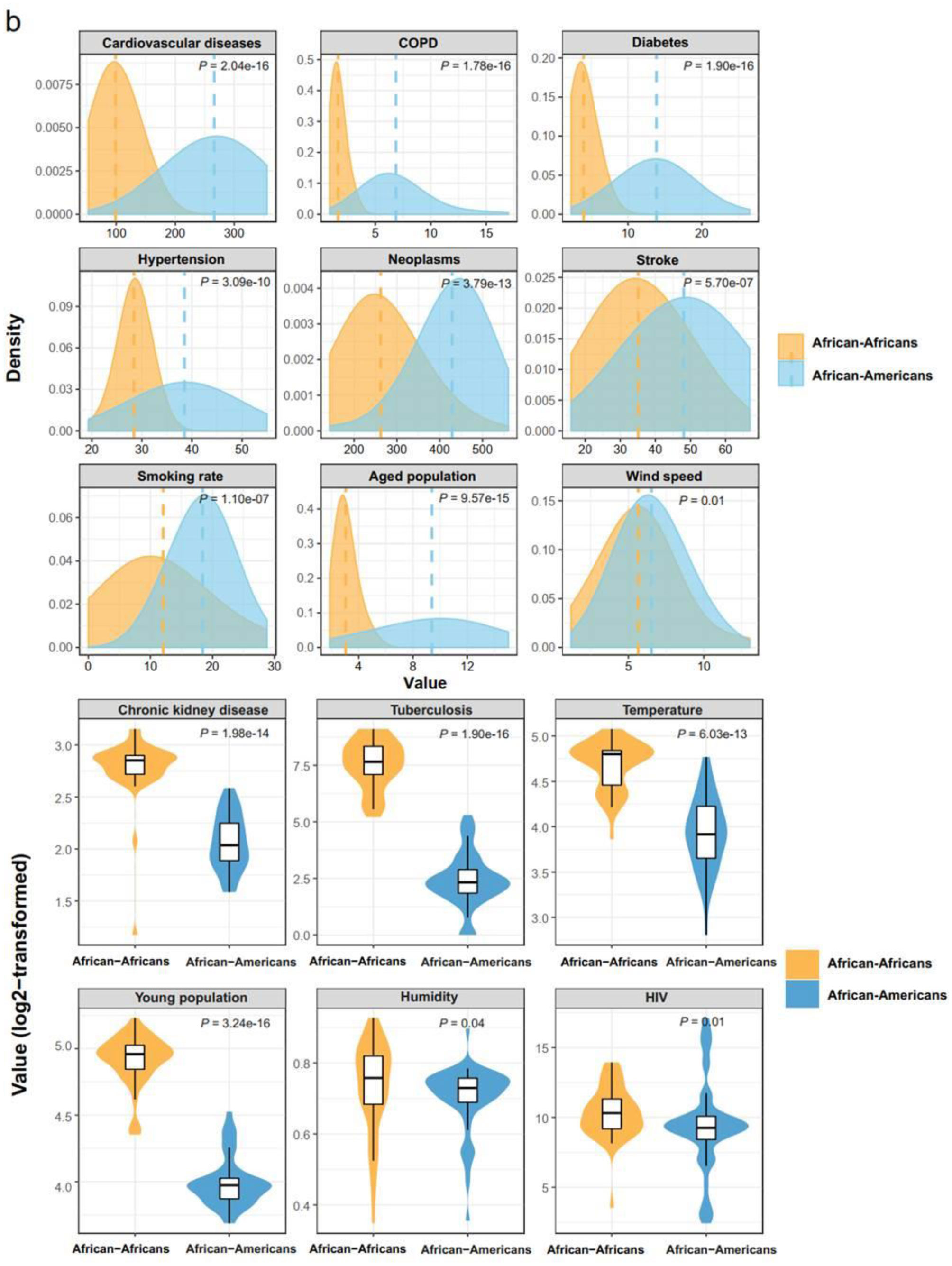
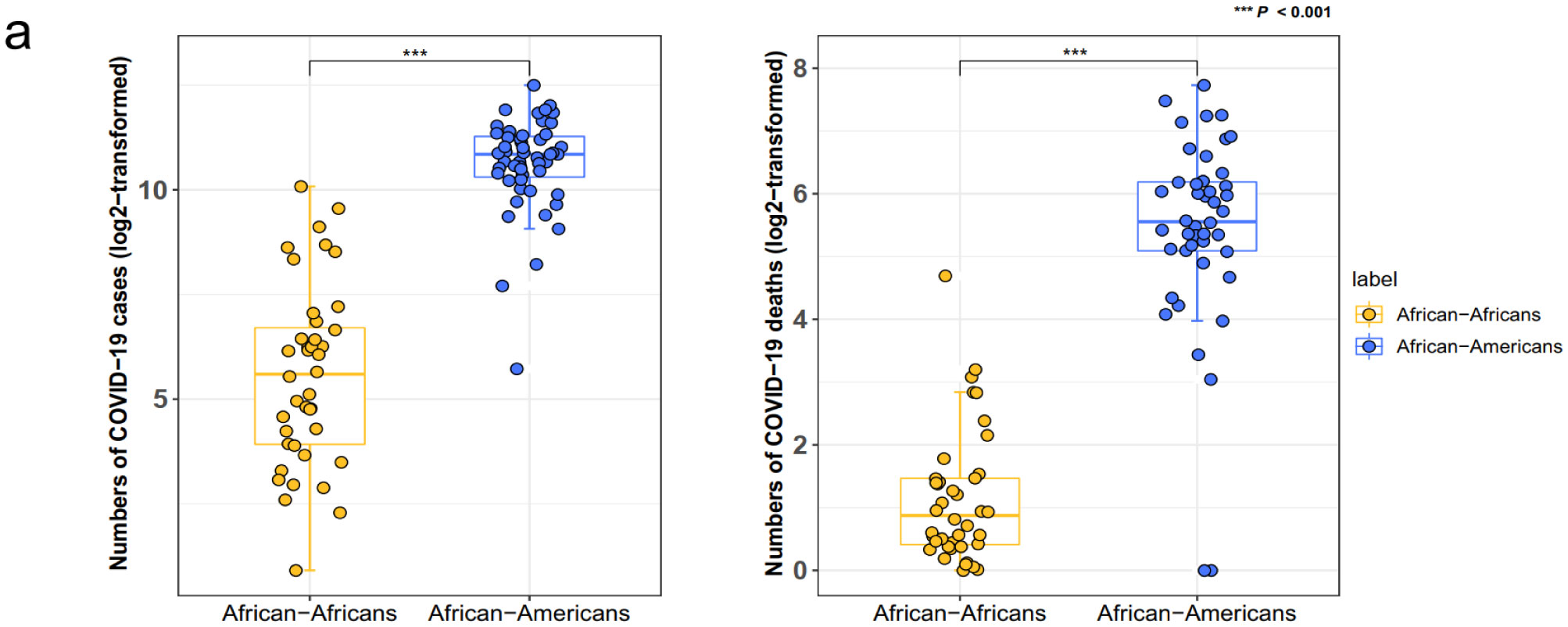
We found that African-Africans had significantly fewer COVID-19 cases and deaths than African-Americans (one-sided Mann–Whitney U test, P < 0.001) (Figure 1a). To explore the potential factors responsible for the markedly lower prevalence of COVID-19 in African-Africans versus African-Americans, we compared several factors between African-Africans and African-Americans, including the incidences of cardiovascular diseases, chronic kidney disease, chronic obstructive pulmonary disease (COPD), diabetes, HIV, hypertension, neoplasms, stroke, and tuberculosis, smoking rate, percentage of aged population (≥65 years), percentage of young population (<10 years), humidity, temperature, and wind speed. We found that the incidences of cardiovascular diseases, COPD, diabetes, hypertension, neoplasms, and stroke, smoking rate, and percentage of aged population were significantly lower in African-Africans than in African-Americans (P < 0.001) (Figure 1b). Additionally, the wind speed was lower in the African countries than in the U.S. states (P = 0.01). In contrast, the incidences of chronic kidney disease and tuberculosis, temperature, and percentage of young population were significantly higher in African-Africans than in African-Americans (P < 0.001) (Figure 1b). The humidity and the incidence of HIV were significantly higher in the African countries than in the U.S. states (P < 0.05).
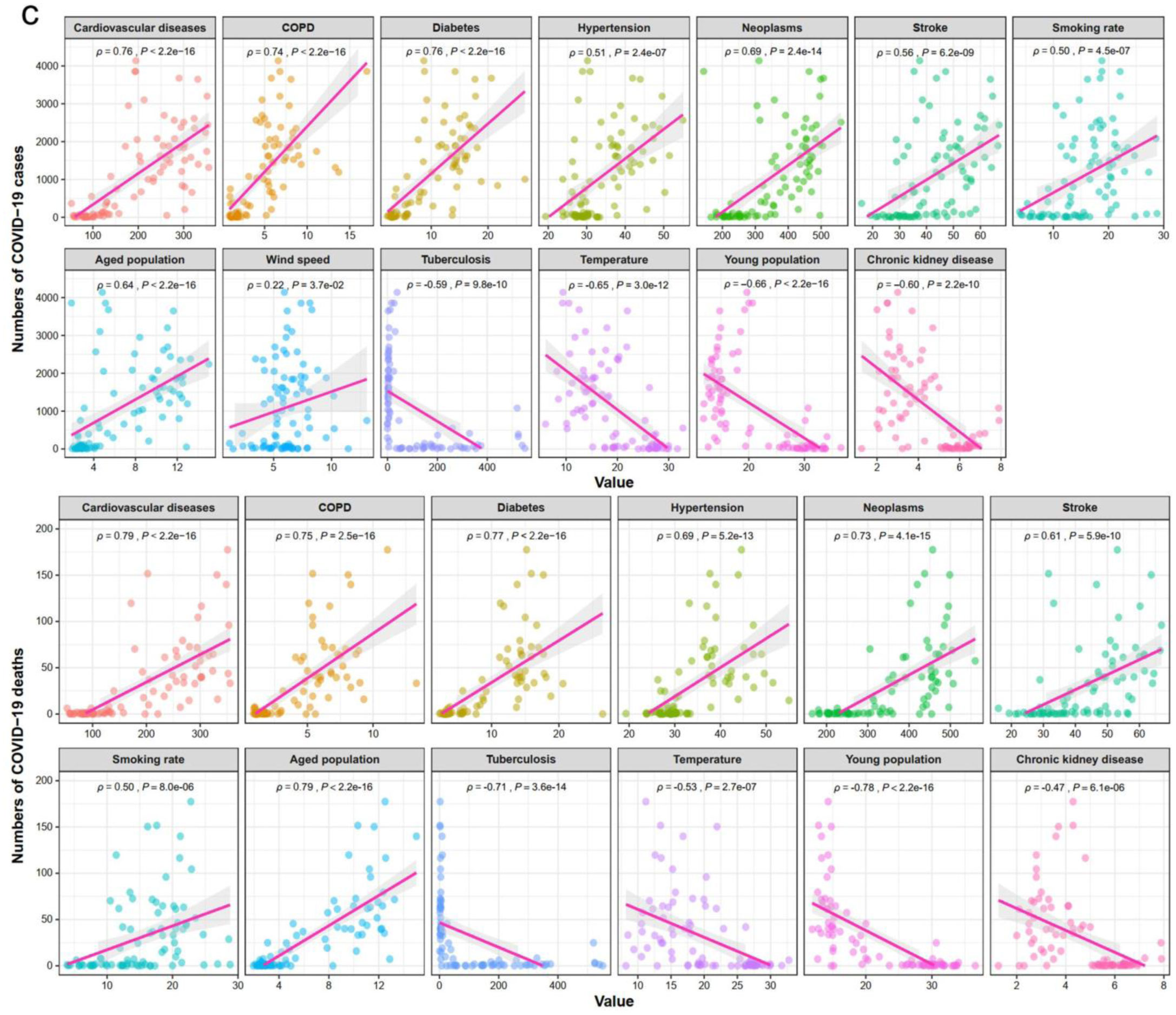
We found that the incidences of cardiovascular diseases, COPD, diabetes, hypertension, neoplasms and stroke, smoking rate, and percentage of aged population were strongly and positively correlated with the numbers of COVID-19 cases and deaths (Spearman correlation coefficient ρ ≥ 0.50) (Figure 1c). Additionally, wind speed had a significant positive correlation with the numbers of COVID-19 cases (ρ = 0.22) (Figure 1c). In contrast, the incidence of tuberculosis, temperature, and percentage of young population were strongly and negatively correlated with the numbers of COVID-19 cases and deaths (ρ ≤ −0.53) (Figure 1c). The incidence of chronic kidney disease had significant negative correlations with the numbers of COVID-19 cases and deaths (ρ ≤ −0.47). Collectively, these results indicate that old age, smoking, high wind speed, and age-related diseases (such as cardiovascular diseases, COPD, diabetes, hypertension, neoplasms, and stroke) are risk factors for COVID-19, while chronic kidney disease, tuberculosis, young age, and high temperature are protective factors. The protective role of tuberculosis against COVID-19 could be attributed to the cross-reactive immunity between other types of infections and SARS-CoV-2 infection [4].
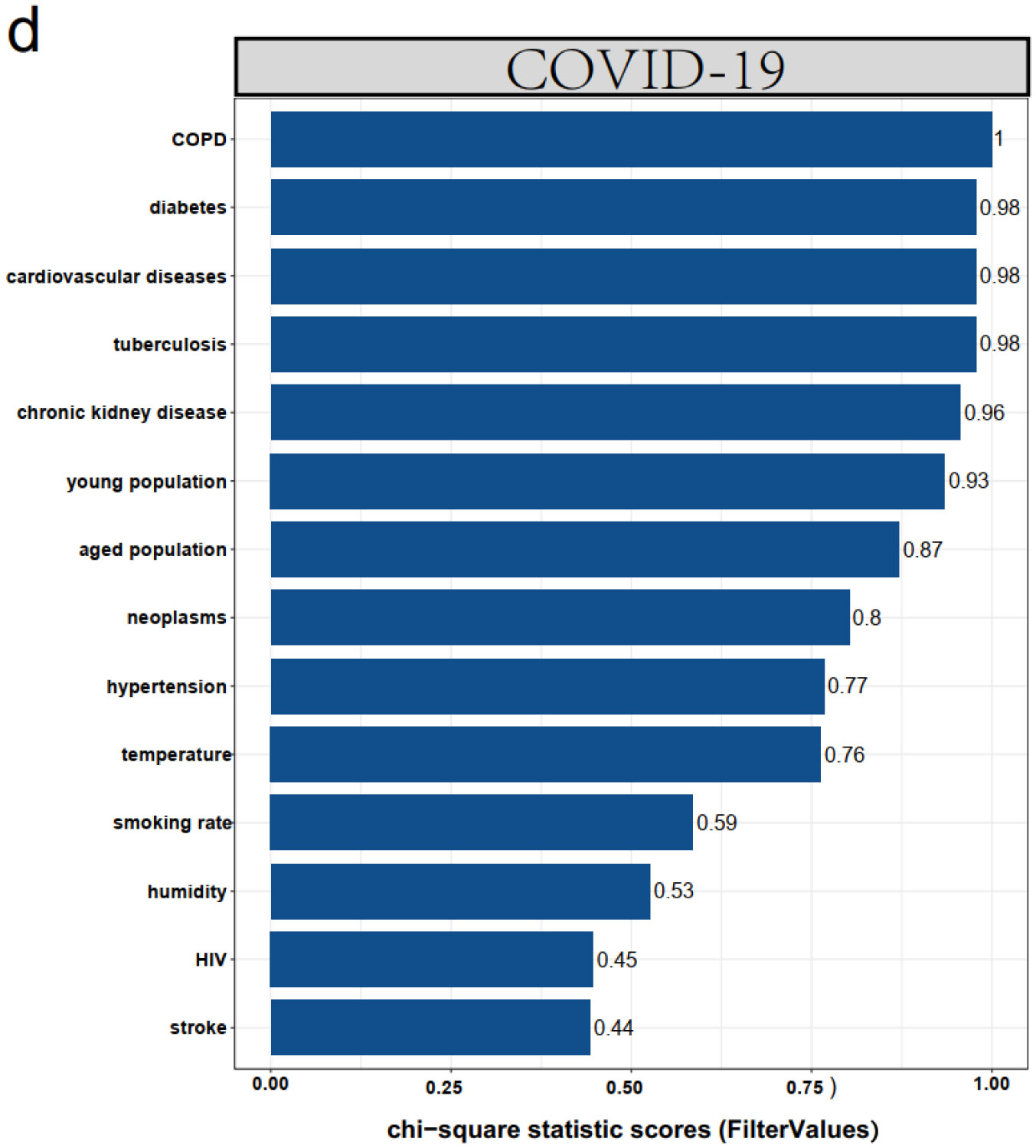
Based on the chi-square statistic [5], we ranked the importance of these factors in distinguishing between the group (African-Africans) with a lower COVID-19 risk and the group (African-Americans) with a higher COVID-19 risk. The COPD was the most important factor (FilterValue = 1), and the next were diabetes, cardiovascular diseases, tuberculosis, chronic kidney disease, and young population (FilterValue > 0.9) (Figure 1d). The aged population, neoplasms, hypertension, and temperature had the medium importance (FilterValue > 0.76). The importance of smoking, humidity, HIV, and stroke were relatively lower (FilterValue < 0.6). Collectively, these results suggest that the age-related diseases and lung diseases are the most important factors responsible for the COVID-19 risk.
4.
Discussion and conclusions
In this study, we investigated diverse factors that could explain the markedly different prevalence of COVID-19 between African-Africans and African-Americans. We found that old age, smoking, and age-related diseases (such as cardiovascular diseases, COPD, diabetes, hypertension, neoplasms, and stroke) were potential risk factors for COVID-19, while chronic kidney disease, tuberculosis, young age, and temperature were potential protective factors. The risk factors of old age and age-related diseases for COVID-19 have been revealed in many previous studies [6]–[8]. The positive association between smoking and COVID-19 risk conflicts with some previous studies showing a negative association between smoking and COVID-19 risk [9]–[11]. However, the evidence for demonstrating the negative association between smoking and COVID-19 risk in these previous studies remains controversial [12]. It is surprising to for us to find that chronic kidney disease is a potential protective factor for COVID-19. A possible explanation could be that chronic kidney disease results in reduced plasma angiotensin-converting enzyme 2 (ACE2) activity in patients [13], while elevated ACE2 expression is a risk factor for COVID-19 [14].
This study has several limitations. First, we did not take into account the intervention measures taken in different countries or regions in analyzing associations between these factors and COVID-19 prevalence. Currently, the effective intervention measures mainly include vaccine injection and social distancing. This study was based on the epidemic data on September 3, 2020, when the COVID-19 vaccine had not been developed. Besides, neither American nor African countries had taken strict measures to control the spread of COVID-19. Thus, both intervention measures (vaccine injection and social distancing) do not appear to have a significant difference between African-Africans and African-Americans. Second, we analyzed the association between a single variable and COVID-19 individually without taking into account the potential mutual relationships between these variables. As a result, the significant association between certain factors and COVID-19 could not be authentic. Third, some other factors, such as ecological factors, which could have impacts on COVID-19, were not included in this study. In conclusion, the significant differences in the age distribution, the incidences of age-related diseases, lung diseases, and HIV, smoking rate, temperature, and humidity could explain the marked differences of COVID-19 risk between African-Africans and African-Americans, although some of these results should be cautiously read.









 DownLoad:
DownLoad: