1.
Introduction
Integration of distributed renewable energy resources (DRER) and distributed energy storage devices (DESD) to the power system networks urges enhanced power electronic solutions [1]. Microgrids are one such application that makes use of power electronics converters. Microgrids facilitate increased integration of DRER and DESD to the power network. This reduces network congestion, improve the efficiency and reliability of the utility network [2,3]. Control requirements of the microgrids require additional power electronics converters to be interfaced to the medium voltage (MV) grid if the conventional low frequency transformers (LFT) are used [4,5,6].
The solid state transformer (SST) is identified as the newest member of the FACTS devices that incorporates multiple power conversion stages providing galvanic isolation with the use of a high frequency transformer (HFT) [7,8]. Compact structure of HFT makes it a good option to replace the LFT [8]. The 'intelligence' or the 'smart' feature of the SST is added by its controllability due to the power electronics interface [8]. In addition to the conventional features of LFT such as isolation and voltage conversion, an SST achieves better power management and power quality [3,4,6,7]. Active power flow control, reactive power compensate ion, voltage regulation, power quality improvement, and fault current limiting are the other SST functionalities that can be integrated into a microgrid [6,9,10,11].
In [11,12], SST technologies, and concepts for power distribution system are reviewed while [13] presents an analysis of SST topologies and controllers. In [14], applicability of SST for traction and smart grid systems with possible modular topologies, existing SST prototypes and their schematics are presented. In this paper, we contribute in reviewing how the SST achieves the requirements of microgrid system for the future distribution network, and the possible design and control architectures for integrating microgrids with the SST. Advantages and disadvantages of each control and design architectures are also reviewed. Existing SST based systems are reviewed to investigate on how far the envisioned SST based microgrid systems have moved towards practical implementation.
The paper is organized as follows. In Section II the applicability of SST for microgrids and how the demanded requirements of the microgrid are satisfied by the SST is discussed. Section III introduces possible and existing architectures for integrating an SST to a microgrid along with a classification. The advantages and disadvantages of each architecture in the implementation point of view are covered under this section. Basic power flow control of a SST and the control strategies adopted in SST based microgrids are reviewed in Section IV. Furthermore, the coordination of SSTs with multiple AC/DC converters is discussed under Section IV. Section V presents three major experimental setups which demonstrate the SST microgrid concept in implementation as prototypes. The paper concludes with suggestions for possible future research directions.
2.
Applying SSTs for microgrids
Integration of SSTs for microgrid applications for improved capabilities have been a popular area of study recently. In addition to the microgrids, the possibility of integrating SSTs with traction systems [18], DRER [19,20,21] and substations [22,23] are also discussed in the literature. The architecture and the control capabilities of SST facilitate the implementation of the microgrids.
2.1. Why SSTs for microgrids
As presented in Table 1, there are several key requirements in a microgrid conforming to the context of the future power system [2,3,11]. Newly demanded performance and functionality requirements of a microgrid given in Table 1 cannot be fully covered by the conventional electric power supply concept based on LFT [11]. Therein, SST based microgrids have emerged as a desirable solution to accomplish these stringent performance requirements as explained below.
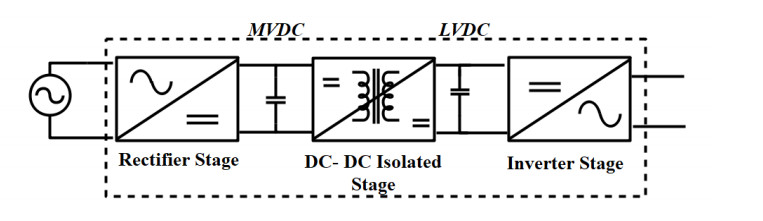
The functional block diagram of the three-stage SST is shown in Figure 1. AC-DC stage (rectification), DC-DC stage (isolation) with HFT and back end DC-AC stage (inversion) constitute the three-stage SST [11]. The presence of multiple ports in the three-stage SST is an attractive feature for the microgrids. The low voltage DC (LVDC) link can be used to directly integrate the DRER, DSED or DC loads. Depending on the voltage levels DC/DC converters are to be used whenever necessary. The DC microgrids are more beneficial than AC microgrids in terms of the efficiency, provided that the system employs DC loads, hence fewer conversion stages. With the recent developments of power electronics converters, large part of the domestic appliances such as computers, LED lightings, televisions, and sensors can be used as direct DC applications. Furthermore, refrigerators, machine drives, and induction cooking systems need variable frequency and are connected to AC through an inverter. For a microgrid serving both AC and DC devices such as a hybrid microgrid, the multiple ports are highly advantageous. Compared to a conventional hybrid microgrid, which needs multiple conversion stages to integrate to the grid, SST acts as a central hub to interconnect both AC and DC devices.
The LFT being a passive interface between high voltage and low voltage system, power quality disturbances such as voltage sag/swell and harmonics at one side of the transformer will easily affect the other. An SST interfaced microgrid is expected to improve the power quality of the system by mitigating those issues [15,16,17].
The first stage of the SST, i.e., the rectifier stage is responsible for regulating the voltage of the medium voltage DC (MVDC) link. This ensures the input of the DC-DC stage is constant. Additionally, the rectifier control system ensures the input AC is in phase with the voltage, allowing a unity power factor. The rectifier control is also responsible for mitigating the harmonics flowing to the upstream of the network by ensuring that the input currents have a sinusoidal shape. However, the harmonic content level is governed by the bandwidth of the PWM controller, which in turn is depended on the SST switching frequency [10]. The SST incorporated at higher voltage levels in the case for replacement of a distribution transformer can be designed with multilevel modular cascaded topologies. The multilevel rectifier at the front end reduces the harmonic injection to the system further [20]. Although the quantitative analysis shows that the on-load tap changers (OLTC) equipped for LFT can perform similar functionality in voltage regulation, a number of tap movements should be incorporated to follow variations in the voltage accurately.
The HFT is the main component of the DC-DC converter, which provides the voltage transformation through medium frequency (power frequency) to high frequency isolation between the main grid and the microgrid [24,25]. Hence, anomalies and the faults encountered in any side are isolated from propagating into the other side. The High Frequency (HF) isolation of the SST results in a less weight and volume when compared to the traditional power transformers [26]. Low weight and volume of the SST make it a good option for applications where weight and space are limited. Nonetheless, the increased frequencies affect the winding and core losses and ultimately in the cooling system. Therefore, the optimizing of the frequency and the size of the transformer based on core and winding material is a major concern in the practical implementation of the SST [26]. The selection of the magnetic materials for the construction of the core and the windings of the HFT are important design considerations [26]. The leakage inductance of the HFT acts as the energy buffer for the power flow of the SST. The power flow control of the SST depends on the high frequency magnetic link and is discussed in section 4.1.
The rectifier control compensates the reactive power injected to or absorbed from the grid. The reactive power control of the SST is hence governed by the rectifier. The DC link in MVDC side of the DC-DC converter affects the input voltage ride through and mitigate the voltage swell or sags from the grid; i.e. when a sag occurs, the MVDC link capacitor injects the accumulated energy and when the swell occurs, it absorbs the excess energy, so that the load voltages are not affected. Since the rectifier stage supplies a constant voltage at the MVDC link, the controller of the DAB acts in maintaining a regulated DC output voltage at LVDC by allowing the required power flow facilitated by the leakage inductance of the HFT.
The SST can be employed to interrupt fault current in the event of a fault on either side of the SST. In the event of a fault, the power electronic switches are turned off and the current flow will be interrupted. The short circuit fault currents in the downstream network of the microgrid strongly depend on the SST controllers. Hence, the fault currents can be reduced and eliminated in a very short time by protection function in the SST [20]. Two basic operating modes of the microgrid are SST enabled mode and the islanding mode. If the DESD connected to the SST based microgrid has sufficient capacity, the microgrid can operate in islanding mode. The islanding mode is enabled by switching off the SST, allowing the microgrid to operate independently from the SST. The DESD of the microgrid starts regulating the DC bus voltage in this mode. The features discussed above can be achieved by designing the SST with proper architecture [27] and a control scheme [28]. In addition, communication enabled SST enhances the operational benefits of the microgrid [10].
The requirements of an envisioned microgrid system for the future distribution network are fulfilled by SSTs. At the same time, it is worthwhile to mention the design and control objectives that the SST should fulfill to enable the interfacing with a microgrid. The major design and control objectives are (ⅰ) bus voltage regulation (ⅱ) power flow control (ⅲ) battery SoC management (ⅳ) power quality improvement (ⅴ) power factor improvement. In addition, energy management and fault isolation are also expected as improved control capabilities.
2.2. Challenges on interfacing SST in a microgrid
Addressing stringent requirements of the microgrids in terms of power and energy management, improved controllability and enhanced coordination is quite challenging. Especially the microgrid architecture and power electronic converters adopted have a significant influence in this regard. For example, as reported in [29] and [30], the DC line losses in two different AC/DC hybrid microgrid topologies are 24% and 56%. The variation is due to the placement and type of power electronic converters used in the two topologies. However, a quantitative/qualitative analysis of the 'SST based microgrids' for these challenges has not yet been done. Table 2 presents the summary of the identified set of challenges and proposed solutions in interfacing SSTs into microgrids.
3.
SST based microgrid architecture
The three ports of the SST can be utilized to form different topologies, and are used appropriately depending on the application interface. The SST can be used both at the LV interface or at the MV interface. Applications of SST in LV interface are the integration of DRER and DESD at LV residential systems [17,20]. Applications of integrating SST with MV involve replacement of distribution transformers such as interfacing microgrids, at substations and in traction systems. At MV ratings and high power applications insulated gate bipolar transistors (IGBT) and HFT are not readily available. In order to solve this problem, a modular and multilevel topologies of MV power converter technologies are employed [41,42]. The MV converter technologies can be used in formulating various topologies of the SST.
SST based microgrids being the focus of this review different SST architectures which are possible for the implementation of single and multiple microgrids are presented in this section.
3.1. Basic SST topologies
There are three basic SST topologies: (ⅰ) Single stage without a DC link (ⅱ) Two stage with either LVDC or MVDC link and (ⅲ) Three stage with both MVDC and LVDC links [5,17].
Single stage SST is the low-cost SST option, with direct AC-AC conversion. Fewer conversion stages imply its increased. efficiency and improved reliability. It is mostly suited for size critical applications. Four quadrant power devices are needed for the bi-directional operation of the converter [17]. Similar to an LFT, the disturbances on primary are replicated on the secondary side.
In two-stage SST, there is a DC isolation stage, either in the LV side or MV side. For high voltage applications, two-stage SST is not suitable, since zero-voltage switching (ZVS) has to be guaranteed due to the wide input range [17]. This topology has a straightforward application in the integration of renewable energy resources [5]. Three-stage SST is the most commonly used and preferred topology in the field because of its high flexibility and controllability.
It has sufficient options to optimize the performance in terms of efficiency and weight/volume. It allows separate control of voltage and current at each stage [11,14,17,42,43,44]. Many attractive features such as reactive power compensation, voltage sag compensation, bidirectional power flow, and DER and DESD integration can be achieved using this topology [4]. A well-known example for three-stage SST is the UNIFLEX SST proposed for smart grid applications [10].
3.2. Modular multi-level converter topologies
For medium voltage and high power applications, the SST cells should be connected in series or parallel, in a modular structure due to the existing limitations in power electronic devices and magnetic materials [45]. In the microgrid application or any distribution system application, SST has to step down the voltage. Therefore, the high-voltage (HV) inputs of the SST modules are connected in series, and the LV outputs are connected in parallel as in the input series output parallel configuration [46]. However, these topologies use increased number of switches, resulting in increased complexity and power losses [20]. For the AC-DC rectifier stage, half-bridge and full-bridge configurations are possible as a topology in one module [47]. Half-bridge module with two transistors can get two output voltage levels, and a full-bridge module can give three possible output voltage levels enabling the AC-DC as a modular multi-level converter (MMC) [47].
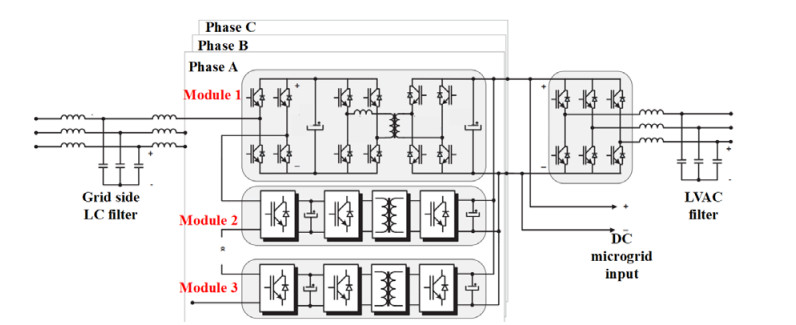
For the DC-DC stage, DAB and the series resonant converter (SRC) can be used. In SRC, the switching frequency operates near to the resonant frequency reducing the losses, hence giving high efficiency. However, inability of SRC to operate in multilevel voltages and to decouple the MV and LV negate the advantages offered by the SRC. Hence, the DAB is preferred [29,47]. Figure 2 depicts a three stage and three phase modular SST topology for microgrids, which is the commonly used MMC topology [6,9,19]. Tri active bridge (TAB), quadruple active bridge (QAB), and penta active bridge (PAB) are known as multiple active bridges (MAB) sharing a common high frequency magnetic link [29,47,48,49]. All these topologies are capable of providing bi-directional power flow, a required condition for the interconnection of a microgrid [42,29]. Having MAB with a shared HF magnetic link improve the cross-coupling power transfer capability, better harmonics performance, and a low current stress on the LV inverter [49].
In considering grid applications of SST, a quantitative analysis is carried in [8] to select the most appropriate DC-DC converter for the SST based on its efficiency. In [8], possible DC-DC converter types including the DAB, SRC, and QAB are compared. The QAB having the highest efficiency and reliability with the low cost is selected as the best qualifier for the DC-DC stage of the SST though its controllability is low [8,48]. In applying SSTs in microgrids, MMC can be used either in the MVAC-LVDC conversion, at the DC-DC stage or at both conversions. However, it is not necessary to use a MMC at the inverter stage since it deals with lower voltages. Nevertheless, in some applications, MMCs are used at all three stages of the SST such as at the 300 kVA UNIFLEX SST [10].
A 20 kVA SST is proposed in [50] and the MMC is used at the front-end rectifier and at the DAB. Also, the MMC has been adopted for both rectifier and the DC-DC conversion stage for a three phase SST in [6,9,14,19]. Depending on the voltage interface of the SST and the power handling requirement, a desirable topology can be selected. In [42], six types of selected modular SST configurations based on its implementation are discussed. The configurations considered in [42], being bi-directional, they satisfy the minimum requirement to replace an LFT in an active distribution system. The advantages and disadvantages of each configuration are summarized in Table 3.
3.3. Architectures for SST based microgrids
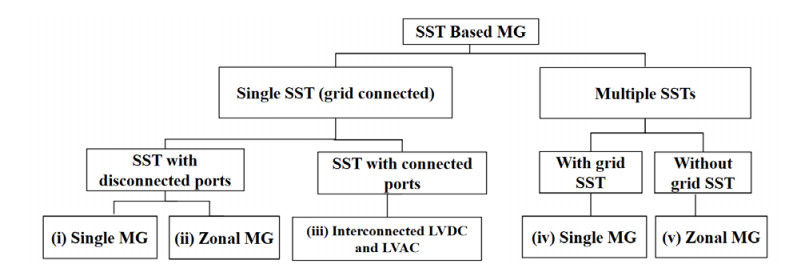
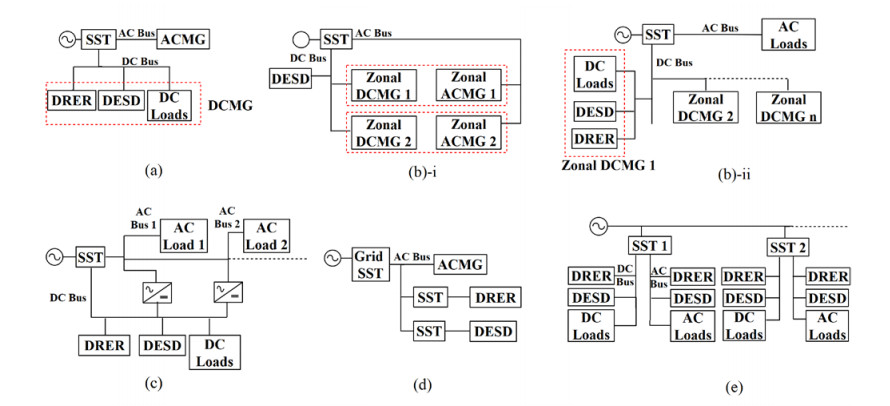
The SST based microgrid architectures can be basically divided into two types: microgrids with single SST and, microgrids with multiple SSTs. Based on the existing and possible SST microgrid configurations the architectures are classified as shown in Figure 3. In Figure 4 this classification is further illustrated. All configurations presented in Figure 4, assume a three stage SST topology and the DC/DC converters are not indicated wherever necessary. The microgrids with single SST, known as the 'grid SST' are usually coupled to the grid. Single SSTs are of two types: LVDC and LVAC connected type, and the disconnected type. The most common and the general architecture is the SST LVDC and LVAC disconnected type and, it has several variations depending on the number of microgrids connected, i.e. Type (ⅰ)—Single microgrid with DESD, DRER and loads (Figure 4a) and Type (ⅱ)—Zonal microgrids (Figure 4b).
Type (ⅰ) has the simplest architecture and control scheme. It has the possibility of integrating an AC, DC or hybrid microgrid. Multiple reverse conversions in an individual AC, DC microgrid are reduced [17]. The Type (ⅱ) is a novel concept presented in [15,53,54] for zonal microgrids and can be implemented in a DC microgrid or DC/AC hybrid microgrid; hence it should be supported with additional power management capability. Due to the interconnection of ports, it has drawbacks of having the requirement of complex communication and control between microgrids [15].
The Type (ⅲ)—SST LVDC and LVAC interconnected concept is presented in [55] and is illustrated in Figure 4c. This architecture offers the advantages of reduction in LV converter size, distribution losses, and converter losses. Due to the interconnection of the DC and AC bus, the voltage regulation is improved in the system. The existing microgrid architectures having multiple SSTs can be divided into two forms: as with and without grid SST. The SSTs can be directly interfaced to DRER or DESD [20,56].
Type (ⅳ) is a multiple SST architecture with a grid connected SST that can be integrated with source and storage SSTs as well as with the AC microgrid as presented in Figure 4d. With this architecture, a decentralized control can be employed. In [21], same architecture is used without the grid SST, where the SST has interfaced a wind generation. It is shown that the DG hosting capacity has improved to 60% with the use of SST. The control being a challenge, there are many research focusing interfacing the large-scale wind generation with SST [21]. With Type (ⅳ) architecture, large DGs can be interfaced to the distribution network. In this scenario, since the SST has to operate in much lower voltages, the option of MMC can be omitted.
The Type (ⅴ) microgrid without grid SST has an SST at each separate zone and is shown in Figure 4e [3]. This architecture is proposed by the Future Renewable Electric Energy Delivery and Management system (FREEDM) researchers. The control is complex and hence, hierarchical strategy is proposed [17,55,57]. This architecture is useful only for large regional networks.
All the above architecture types can be categorized in terms of energy storage as well, i.e. with a common DESD or each zone/SST having a separate DESD. For example, as denoted in Figure 4b-i, the Type (ⅱ) mentioned above can have a central DESD with multiple Zonal microgrids and each Zonal microgrid can have a separate DESD.
In [35], a novel resilient SST based microgrid design having two separate LVDC and MVDC microgrids is proposed. In this system, storage is connected to the LVDC but, with a potential to be connected at the MVDC whenever required. This design is not included in the categorization. Using centralized storage is a cost-effective option to trade off the high cost of zonal microgrids. The stability issues of the multiple SSTs connected to the grid, especially to a weak grid, needs to be further researched and corresponding damping techniques need to be investigated [24].
4.
SST based microgrid control
The performance of SST based microgrid mainly depends on the control algorithms of the SST(s). For the reliable operation of a microgrid, power control scheme should be capable of operating under different modes and conditions of operation.
4.1. Power flow of the SST
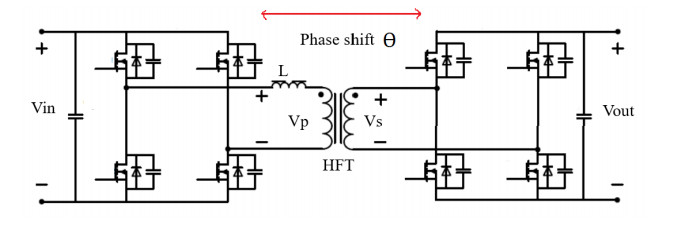
The three stage SST, topology by design allows the bi-directional power flow, the major requirement of a microgrid. The front end rectifier (see Figure 1) is responsible for regulating the voltage of the MV DC link, shaping the input current; thus achieves the reactive power compensation and harmonic elimination [13]. In the second stage of the three stage SST; the DC-DC converter controls the power flow across the SST and regulates the LVDC bus voltage. The most commonly used architecture for the DC-DC converter is the DAB, which is controlled using phase shift modulation (PSM) also known as single phase shift modulation (SPSM) [25,49]. It uses the phase angle of the primary and the secondary of the HFT to control the direction and the magnitude of the power flow. The amount of power flow from one bridge to the other bridge is controlled by adjusting the phase shift between the primary and the secondary voltage waveforms of the HFT. The power flow of the DAB is given by (1) where Vin, Vout are the input, output voltages of the DAB, Ɵ is phase angle displacement of the input voltage and output voltage of HFT(with a unity turns ratio), f is the switching frequency and L is the leakage inductance of the HFT. Ɵ is controlled to generate the switching signal using PSM. When Ɵ is zero, there is no power flow in the converter. When Ɵ > 0, power flow direction is towards the microgrid from the grid and when Ɵ < 0 the power flow towards the grid from the microgrid [25]. DAB power flow is illustrated in Figure 5.
However, the SPSM can only manage the average output power, because it has only one degree of freedom. The Equation 1 can be rewritten with the duty ratio D, as expressed in Eq 2 [49].
Another modulation scheme applied for DAB and other MAB topologies is the dual-phase-shift modulation (DPSM) with two degrees of freedom [49]. In addition to the phase shift between the primary and secondary side, it controls the phase-shift between half-bridges in the identical sides [49]. This is represented in Eq 3 where D1 and D2 denote the inner phase shift and the outer phase shift ratio of the DAB [49].
For other MAB topologies, the transferred power from the SPSM and DPSM is presented in [49]. The control loop of the DC-DC converter guarantees the LVDC bus voltage regulation and permits the variation of the power flow. The voltage source inverter regulates the LVAC bus voltage required for the AC microgrid. The controllers for each stage of the SST are discussed under decentralized control.
4.2. SST based microgrid system control
The control environment of a microgrid is both time-varying and complicated. For example, the intermittent nature of the DRER always varies with the power output to the microgrid. Not only DRER but loads and the DESD are also time-varying components. Reference [14] presents the main control objective of such a microgrid system. To maintain the power balance, the power consumed by loads of AC and DC microgrids, PLOAD should be equal to the sum of the power supplied by the SST, PSST, power supplied by the sources of the DC microgrid, PDC_MG and the AC microgrid, PAC_MG. This is represented in Eq 4.
The SST based microgrid control techniques discussed in literature are identified under three categories: centralized control, decentralized control and hierarchical control [54,58,59,60]. Centralized and decentralized schemes have been the common control solution to cater the control requirements of microgrids. However, when considering the challenging control requirements imposed on microgrids, such as operating the microgrid in the islanding mode, optimum battery management and the seamless transfer between the two operational modes, more advanced controlling must be employed. The hierarchical control for SST microgrids was introduced in [44] to address these challenges. The discussion under this section is focused on the system level controls, rather than considering the microgrid device level controls; such as battery control, solar PV control and load control. The below analysis of the control structures is discussed focusing on single microgrid.
In centralized control, the SST becomes the central controller, where the microgrid is linked to it with a communication link. This has the drawback of relying on the communication that degrades the system reliability. Due to the limited capabilities, central control techniques are rarely applied in SST based microgrids. Depending on the control objective, the SST employs either current controlling or voltage controlling.
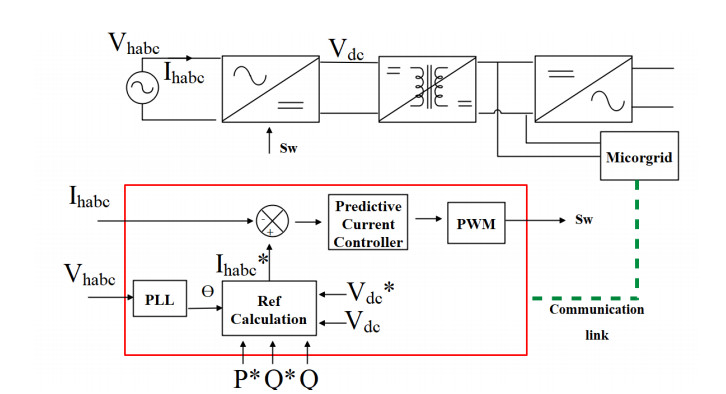
In [10], a predictive current controlling technique for power management is presented for the UNIFLEX system and is shown in Figure 6. Depending on the power requirement of the microgrid measured using remote measurement units, the active power reference, P*, and reactive power reference, Q* are calculated. The controller technique introduced in [10] uses a multi-loop system where both DC bus voltage, Vdc and the power flow are controlled at the same time. The overall control system constitutes a phase locked loop (PLL), reference generators, predictive subsystem, and PWM generator. The current of MVAC side, Ihabc is compared against the reference current, Ihabc* to calculate the switching signal, Sw. In [61], a voltage control algorithm based on fuzzy logic is proposed for the control of the DC-DC DAB driving a constant power load. The proposed fuzzy logic controller (FLC) scheme operates the voltage loop in the fuzzy operation, improving the robustness and dynamic performance of the voltage loop of the DAB. The voltage regulation at load transients is quantified in this study. In [62], a PI control scheme based on two fuzzy networks is designed for a three stage SST. Implementation of fuzzy controllers to fulfill other stringent control requirements is a possible area for future studies. In decentralized control, a local controller exists for each stage/component of the microgrid and the control measurements are taken locally. Decentralized control scheme for SST microgrid provides more simple and robust control capability [10,38,61]. In decentralized control, the converter controllers in the three stages are not linked to each other; hence, it increases the system reliability.
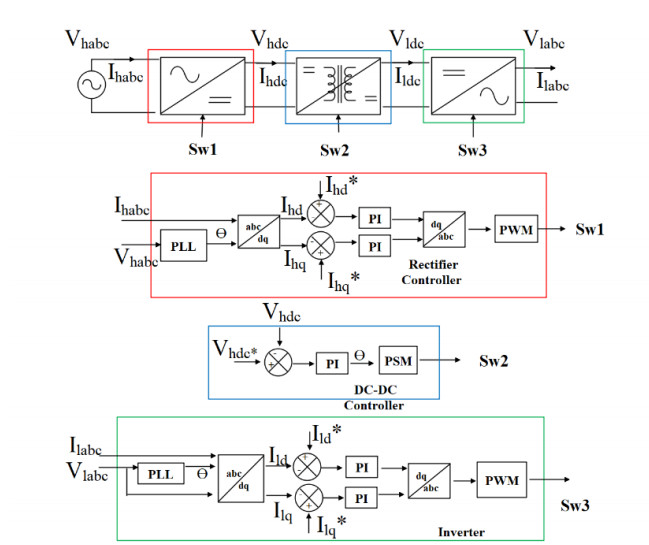
A general control block diagram for the decentralized SST based microgrid control is shown in Figure 7. The PWM signal Sw1 in the rectifier stage is generated by taking the input parameters of the MVAC side of the SST Vhabc and Ihabc. Similarly, the Sw3 switching signal in the inverter is generated by taking the output parameters of the SST Vlabc and Ilabc. Decoupled dq control is used in this generalized control diagram for the rectifier and the inverter stage. The dq axis currents at MVAC and LVAC side of the SST are Ihd/Ihq and Ild/Ilq respectively. The reference d axis currents (Ihd* and Ild*) are calculated by the respective DC bus voltage controller whereas the reference q axis currents (Ihq*/Ilq*) are calculated considering the required power factor (common practice is to set Ihq*
= 0 and Ilq* = 0 so that rectifier and the inverter operates at unity power factor). The Sw2 switching signal is generated according to the PSM.
In [38], a DPSM is employed to manage the power flow, and to balance the module level voltage to prevent the voltage unbalance occurring due to modular multilevel structure. Similarly, in [58], voltage unbalance issue at the capacitor is addressed using a central control scheme based on PI controllers.
Hierarchical control embodies the advantages of both centralized and distributed control; hence, more advanced control objectives can be met [3,44]. Hierarchical control is derived from the ANSI/ISA–95 [54] and operates based on different time scales depending on the control requirement. It has three layers: primary, secondary and tertiary. Centralized and hierarchical power management control strategies for SST based DC microgrid are presented in [44,60]. More complicated hierarchical and distributed control architecture is deployed in FREEDM System Center [3]. Better coordination between different operating levels can be seen in the hierarchical control, and thus makes it highly applicable for the SST based microgrids. In [3], modular multilevel rectifier with DAB with smart microgrid adopts a hierarchical microgrid control. A summary of the control strategies for SST based microgrids is provided in Table 4.
4.3. Co-ordination of SSTs and interfacing converters
The SST based microgrid is a complex system where multiple number of converters are associated. When SST acts as the interface to the main grid, the voltage and power balance of the microgrid system under predicted conditions, is achieved by the SST by its design [35]. However, co-ordination between microgrid converters can achieve more controllability, optimize the system performance, improve power quality and improve network stability [64]. Communication links from the SST to each device of the system are proposed in the envisioned SST microgrid systems in [3,57]. In the presence of a single SST, the SST acts as the main controller, which manages the power flow and voltage control. But, the system becomes complex in the presence of multiple SSTs and microgrids [64] where a coordinated control is mostly preferred. Even for systems with MMC based SSTs [65] or systems which have unpredicted loads and generations [66], coordinated control schemes are suggested. However, SST based microgrid coordinated control is still a possible research area to focus.
Although the research focusing on power management of the SST is popular, SST control algorithm incorporating energy economics is an open topic for research. For example, if the time dependent price of electricity at a particular moment is expensive, power flow to the DSED shall be reduced and vice versa [9]. A controlling mechanism, considering the safe operation of the SST in the grid, still preserving its functionalities is a future focus of SST technology [8].
5.
Experimental prototypes
This section presents, SST based microgrid test systems developed worldwide.
5.1. Future renewable electric energy delivery and management system-FREEDM system
The FREEDM system is an envisioned smart grid proposed with the basis of novel technologies like SST. The FREEDM system is used as a test-bed in many research discussing control and design techniques for SSTs [3,43,44,55,57,60,]. The system architecture employed in the FREEDM system is of Type (ⅴ) introduced in section III. The system consists of multiple SSTs enabled with a fault indication device (FID) and communication [3]. In [3], advanced cascaded control based on 4 control levels; (ⅰ) user level, (ⅱ) SST level, (ⅲ) FREEDM system level and (ⅳ) multiple FREEDM system level is presented. The control objectives at levels 1–3 are (ⅰ) demand management, (ⅱ) DC bus voltage regulation, power management, and power quality maintenance and (ⅲ) fault management and energy management, respectively. Level 4 control coordinates multiple FREEDM systems that form a large regional grid. A hierarchical power management strategy for the FREEDM system is presented in [44,64]. Here, the battery SoC level is managed in the tertiary control for battery management [44]. Hierarchical control strategy used in [44] presents a time dependent intelligent fault management (IFM), intelligent power management (IPM) and intelligent energy management (IEM). In [24], a 3.6 kV–120 V/10 kVA SST prototype is developed and tested with a hierarchical control strategy, which was integrated with the FREEDM center.
5.2. LEMUR project
The LEMUR Project has a 150 kW SST with a DC link (750 VDC) where a DC microgrid is connected, and two AC links (375 VAC, 750 VAC) where multiple nano microgrids are connected. The DC microgrid is connected to the interconnected LVAC and LVDC. The proposed system architecture is of Type (ⅲ) introduced in section Ⅲ. The LEMUR project has recorded an efficiency of 97.17% including the IGBT losses at 100% loading level. It adopts a TAB with centralized controller for current and voltage regulation.
5.3. Highly efficient and reliable smart transformer-HEART project
The HEART project undertakes a modular approach for the 'smart transformer' [8]. In order to approach the challenges of reliability and efficiency, the HEART researchers have used a modular approach. A scaled down three phase SST prototype of 100 kW, 1.5 kV 800 VAC, 800 VDC with a QAB converter is built. It has three cells of cascaded half-bridge at each phase [67]. The main control objectives of the controller are to control the local loads and sources while controlling the voltage of the MV and LV network. In [68], the HEART researchers proposed a soft load reduction method based on the SST similar to the load shedding to compensate the grid instability due to high loading. The developed SST in HEART project was also employed for the replacement of an LFT in a distribution feeder and recorded a 60% improvement of DG hosting capacity in wind generation [69].
6.
Conclusions
Solid State Transformers (SSTs) are most likely to play a key role in the future smart grid. It has been identified that microgrids are a defined market for the SSTs. This paper has presented a comprehensive review and comparison on integration, design and control aspects related to the SST microgrids. Six possible architectures to integrate the SST with microgrids are reviewed and the advantages and disadvantages of each design is presented. SST by design adds voltage and power flow controllability to the microgrid. More advanced control schemes based on device communication can optimize the power flow and energy management and of the network. SST microgrids Experimental setups worldwide are presented with their respective design and control architectures.
The SST by its design, offers multiple advantages to both the utility and the consumer. However, multiple SSTs connected to the grid can cause stability issues, especially in the weak grids, and should be investigated further. In terms of the SST based microgrid control, design of coordinated control scheme between conversion stages for the decentralized control is a possible area for future study. Energy economics, safety and protection considerations, and fault identification of SST based microgrids are other open topics for research. Despite the benefits offered by the SST based microgrids, in terms of the efficiency and the cost, LFT technology still imposes a competing challenge for the SST. With the improvement of Nanocrystalline core and SiC power devices, SST efficiency will continue to improve, enabling more efficient integration. Quantifying the economic benefits of the SST based microgrids, might tradeoff the cost associated with it. More research must be undertaken with regard to the costing and return on investment of the SST microgrids.
However, with the stringent requirements of the future power system, where DC loads and sources will become plug and play devices on the residential environments will notify the boost of SST based microgrids. Thus, the design and control of the SST microgrids will continue to evolve as a collaborative challenge for the power electronics and power systems engineers.
Acknowledgments
Authors would like to acknowledge the financial support provided by the University of Moratuwa, Sri Lanka under the research grant SRC/ST/2019/39.
Conflict of interest
The authors declare no conflict of interest.









 DownLoad:
DownLoad: